Telehealth is slowly being integrated into the healthcare delivery system worldwide. Communications dealing with organisational challenges, human resources and deployment of Management science in initiating, sustaining and making viable telehealth activities are few. This article shares the author’s learnings over 22 years of association with a number of small and mega telehealth projects operational in India and overseas, virtually reaching the unreached.
A detailed need assessment study is the first step in this direction. Risks in programme implementation, challenges in providing tele consultants, necessity for training, retraining, learning, relearning and unlearning has to be considered. Identifying champions in the team and community and making the project self-sustaining is critical. Future-ready access to cost-effective, need-based, appropriate technology including a robust telecommunication network is vital. Patient perspectives of telemedicine quality need to be considered. Measurable, reproducible, objective parameters quantifying success need to be defined. Legal, regulatory and security issues have to be complied with. Cultural transformation is necessary for acceptance of technology enabled remote virtual healthcare. Urban teleconsultants deploying cutting edge technology need to be sensitised for community interaction. Implementing pandemic associated specific strategies and providing equitable, quality, accessible, affordable healthcare, in a milieu of infrastructure and personnel shortage, is always a challenge.
The need assessment team interacted with all stakeholders including administrators, doctors, district health officials, patients and the community. Clinical problems were identified. Beneficiaries, at the "bottom of the pyramid" had to interact with urban super specialists. Challenges included (a) convincing the community that an urban healthcare provider could appear on a screen, make a diagnosis and advise treatment empathising with them (b) convincing doctors at the remote centre, that the new service would not undermine their importance (c) convincing government that a radical exponential cultural transformation could be implemented and the programme would be cost effective using appropriate need based technology and (d) Programme Managers would be transparent, accountable, responsible and open to external third party audit. Managerial decisions were reviewed in real time and corrective measures instituted.
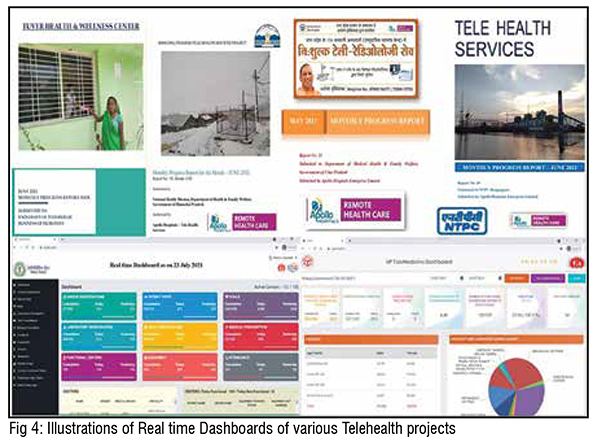
Acceptable, clear, unambiguous, reproducible, measurable parameters to decide on what constituted success were defined. Quality of service was measured through feedback. Key Performance Indicators were defined. Channels of communication and grievance redressal mechanisms were instituted. Escalation and evaluation matrices were customised. Internalisation of processes and protocols enabling smooth functioning was ensured with constant training. Training, capacity building, CME programmes, weekly and monthly project reporting, efficient community engagement and optimised capacity utilisation were implemented. Monitoring and evaluation included impact assessment study of measurable milestones and monthly reports. Program management included budgeting and defining Service Level Agreements (SLA) for all activities. This included data bandwidth SLA for Service Providers and penalties for Service Commitment outage.
Training was carried out for staff and government employees in (a) Clinical areas, (b) Information Technology (IT) (c) Attitudinal Change (d) Community Linkage and (e) creating beneficiary delight. Change management and workflow process re-engineering were new areas. A new workflow process was integrated into the existing government healthcare system. An intensive threemonth training was given [Figure 1], for Telehealth Coordinators / Facilitators. Training covered basics of telemedicine, telemedicine equipment, IT for teleemergencies, trouble shooting, petty cash accounting, Management Information Systems and reporting and community linkage programmes. Staff were taught to present clinical problems in an emergency setting. A well-integrated teleconsultation unit with remote diagnostic devices (digital 12 lead ECG, Spirometer, Stethoscope, Point of Care Diagnostics) and seamless Internet connectivity, enabled implementation.
Community contact was initiated with resource persons distributing simple, illustrated information booklets in local language. Change management issues were faced with local staff, who initially perceived telehealth as a threat. Technology provided virtual specialists on a screen, but providing drugs and tests was difficult. “Just enough” bandwidth always available, was better than unreliable ideal bandwidth. Redundancy was provided with additional backup.
Technology acceptance was a concern. A resource in each centre was dedicated for community outreach. A detailed Standard Operating Procedure was made. Constant skilling and upskilling ensured use of hardware and software. English speaking translators were made available. Dedicated generators, with adequate diesel ensured constant power. Subsequently, solar panels were introduced. Specialists in quaternary care hospitals, had to provide teleconsults for a token compensation. Younger consultants were more enthusiastic.
Evidence of cost-effectiveness is necessary for widespread telemedicine adoption. Ensuring funding and sustainability is necessary. Donors, governments, cross-subsidy, for-profit companies, and rarely venture capitalists have been sources of funding. Successful telehealth applications are generally run by local telemedicine champions with ad hoc funding. Few have succeeded in reaching large-scale, enterprise-wide adoption. Personal user advantage and incentivisation is as important as advocating general societal advantages.
A telemedicine network is usually a sub-system within an organisation. Telemedicine systems should compute setup and running costs to ensure sustainability Measuring performance is essential, selecting characteristics to be measured, choosing a method to measure, analysing collected data and implementing decisions based on these results. “Performance” criteria would differ for each stakeholder eg. patient, telehealth coordinator, teleconsultant and financial officer. Societal perspectives could be different. Measuring impact should be contextual with appropriate indicators and metrics. Indicators ‘indicate’ impact but do not quantify, whereas metrics are ‘numerical indicators’ quantifying impact. Combination of indicators and metrics is needed. Indicators could include (a) Utilisation (How busy is the network? (b) Quality (how good are responses? (c) Usability (how easy is the system to use? trouble shooting technical problems?) and (d) patient outcomes.

Local champions promote participation, exploiting technological and financial options. Sustainability depends on existing structures and processes in the local healthcare delivery system, policy frameworks, communication and technology costs and physician and patient acceptance. Telehealth service is sustainable when it is part of a healthcare delivery system. Collaboration within the institution, developing community alliances, external partnership, shared vision, exploiting funding opportunities and technological options, identifying critical services, engaging external specialists and improving administrative processes are important. Telehealth iementation requires rethinking and redesigning of functions, structure and culture to achieve improvements in cost, quality, service and speed. Main objectives are developing new business processes supporting and improving service delivery, continually evaluating enterprises structure and operations to achieve more responsive systems. Interpersonal trust, faith in reliable appropriate technology and teleconsultation process is necessary. Use or non-use is determined by social context in which technology is implemented. Collaboration between entrepreneurs, managers, bureaucrats, healthcare professionals and patients is critical. Analysis of beliefs, perceptions and attitudes about telemedicine is important. Solutions should be technologically appropriate and culturally sensitive. Appropriate technology is the simplest solution achieving the desired purpose in existing social, cultural, economic and environmental conditions, promoting self-sufficiency. Such a technology with fewer resources is sustainable. Change management is addressing the human factor, defined as “resistance to change”. Change is the process of switching from “old” to a “new” situation. Individuals are aware of reasons for change, changes that are necessary, details of new technologies, its implementation and new skills required. Most telehealth evaluation studies are technologycentred and focused on utilisation rates. Patient opinions shape marketplace and need to be studied. Healthcare is a competitive industry. Low utilisation rates could be due to poor telemedicine encounter experience.
Telehealth is a major innovation at the technological, social and cultural levels. Telehealth projects are complex, innovative and continually evolving. Some effects cannot be anticipated. Telehealth has a poor record of implementation and adoption. Incentives to health professionals have been suggested to increase telemedicine adoption. Self-sustaining telemedicine applications improve access to healthcare and savings. Rate of adoption is the speed with which a technology is adopted. Importance of introducing evaluation and monitoring, needs to be recognised. Quality Assurance (reviewing reports, monitoring cases/users and checking data) in telemedicine programmes has been stressed.
These include technology integration, interoperability, standardisation, security, time constraints and financing. Technology can be provided, but health professionals need to use it. Their perceptions, legal issues, technical difficulties, time, convenience and cost are critical. Hurdles relate to reimbursement, policies governing telecommunication and information technologies, development and licensure. Difficulties in introducing telemedicine and eHealth have been pointed out. Internal resistance to changes in work processes and organisational transformations are barriers.
Acceptance by clinicians and beneficiaries, demonstrable savings, improved access to healthcare and reduced effort and travel time, adoption into everyday practice are reasons for successful telemedicine applications. Active deployment of Management Science in disruptive innovations like telehealth is limited. Adoption of telemedicine, patient satisfaction and doctor-patient interactions depend considerably on utilisation of Human Management principles. The latter is intuitive The diffusion of innovation (DOI) theory is useful in assessing perceptions about a new technology such as telemedicine. Telehealth adoption is a complex behaviour determined by a large set of psychosocial factors.
If patients perceive that telemedicine will save time/money and increase comfort, they may adopt telemedicine. Pre experience perceptions shape decision to (a) sample telemedicine services and (b) use services regularly. Greater the perceived advantage and perceived compatibility, greater the intent. User advantage determines speed of adoption. Rate of adoption is speed with which technology is adopted. Increased access results in increased utilisation. To ensure effective operation, skilful planning and implementation are as essential, as system design, software functionality and technical prowess. Optimisation of work processes is important. Operations need to be reinvented to use newly available information. Identifying significant pain points results in new innovative solutions. Innovative uses of telemedicine have been reported
The new normal will be predominantly remote healthcare. Physical visits will be for procedures in single speciality hospitals. Personal health records will be updated in real time and stored in the cloud. Individuals will manage their own health with assistance from a nurse practitioner. Smart robots with artificial intelligence (AI) will help conduct or interpret lab tests and other tasks performed at home with networked diagnostic devices. Internet, mobile computing and inexpensive sensors will offer opportunity to democratise healthcare, making the system resilient. Technology enabled care will increase productivity and savings, improving health outcomes. Continuum of healthcare will provide individualised care maximising resources.
Instead of patients moving from remote areas to hospitals, information will move from a centralised area to the patient Digital efficiency should not be at the cost of TLC (Tender, Loving Care). Telemedicine should be a tool to achieve an end, requiring skills in medicine, digital tools, information and communication technology and administration. Telehealth will make healthcare accessible, accountable, equitable and affordable maintaining patient trust. Humankind is witnessing an unprecedented growth in Healthcare Information Technology. Machines will be interacting directly through the World Wide Web (Machine to Machine – or the Internet of Medical Things).
Present human to machine interaction will reduce. With three billion using social networks, distance will become meaningless and Geography History! Remote Healthcare is here to stay. The WFH (Work from Home) culture will be adopted by the healthcare provider and the beneficiary. The future of healthcare, lies in building hundreds of stand-alone, small, satellite clinicians offices and diagnostic centers. Existing hospital-centric focus will shift to patient-centric focus
Scores of individuals have managed various telehealth projects. Dr Prathap C. Reddy Founder Chairman Apollo Hospital Group had realised in 1998 that telehealth would be the future. Dr.Preetha Reddy Vice Chairperson and Dr. Sangita Reddy Joint Managing Director, gave carte blanche to the operational team. Vikram Thaploo CEO is managing an outstanding team of dedicated professionals. S Premanand Chief Business Officer and Dr Ayesha Nazneen Chief Operations Officer among others have overseen dozens of section managers and their assistants who are all part of this extraordinary team facilitating 25,000 e-Transactions every day.